How Variations in Health Systems Influence Oncology Practices
By Ashwin Athri
Changing marketplace dynamics related to the demographics and economics of cancer care is making it necessary for health systems to adapt and invest in capabilities ranging from care coordination models to a sophisticated IT infrastructure. By modeling and quantifying these marketplace dynamics and economic drivers/levers, we can uncover the influence of health system behavior on oncology practices and the local markets. Our analysis across multiple tumor types has demonstrated that health systems are wielding a growing influence on how care is delivered in the local markets in which they operate.
Health care marketplace dynamics are changing rapidly across the United States, especially in oncology. Some of the changes are the result of health systems that have evolved into integrated delivery networks (IDNs) and, in the process, have acquired oncology medical groups. IDNs, in turn, have in some cases sought to leverage those acquisitions to achieve their objectives, including improving margins and attaining quality measures.
Payers have also been working to develop more power and influence over the treatment of cancer by forward integration into specialty pharmacy distribution, adoption of treatment protocols or clinical pathways, and implementation of formularies in order to prefer one oncolytic to another. In addition, there is a wide array of partnerships among payers, distributors, and health systems influencing care delivery (Figure 1).
 As a result of these changes, it is becoming harder to identify where the locus of treatment decision-making power resides in each local market. Along with these systemic marketplace changes, a variety of trends are driving changes in purchasing and prescribing behavior and, subsequently, the health systems’ influence:
As a result of these changes, it is becoming harder to identify where the locus of treatment decision-making power resides in each local market. Along with these systemic marketplace changes, a variety of trends are driving changes in purchasing and prescribing behavior and, subsequently, the health systems’ influence:
- Cancer incidence is expected to rise 45%, with a 30% increase in survivorship (2010 to 2030)1
- Federal payment reform and reimbursement reductions (including 340B) for physician offices have prompted a shift to providing cancer care in the hospital outpatient setting
- With reducing reimbursement rates, “buy-and-bill” drug distribution presents significant financial risk for practices, triggering a shift to hospital-based outpatient infusion centers for infused oncolytics and to in-office dispensing capabilities for oral therapies
- Demand for outpatient chemotherapy continues as treatment regimens grow more complex
- Oncology therapies with newer requirements for specific companion diagnostic tests are prompting more aggressive payer utilization management techniques
- Payers are implementing outcomes/value-based payment models and contracts
Understanding the Impact of Health Systems in Local Markets
By modeling and quantifying these marketplace dynamics and economic drivers/levers, we can uncover the influence that health systems hold over oncology practices and the local markets.
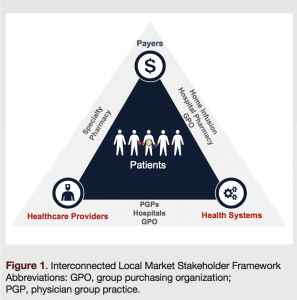
To understand the impact of health systems, we must first understand and define the local markets they operate in. The Dartmouth-defined2 hospital referral regions (HRRs) are a great starting point for the creation of actionable and significant local markets, as these geographic groupings are designed to capture treatment approaches, referral patterns, centers of excellence, and populations specific to each region (Figure 2). Each HRR is further subdivided into hospital service areas that are defined by hospital cities.
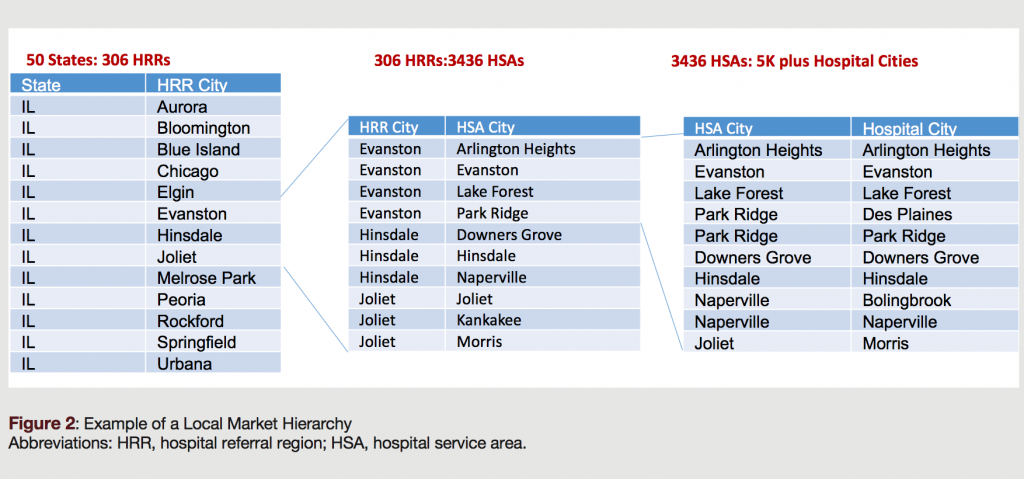
After defining the local markets, it is vital to understnd where the health system players lie on a maturity spectrum. This measure is based on each system’s capabilities, including risk management, care coordination, consolidation, and IT sophistication. At Precision, we have developed a sophisticated IDN Maturity Model that organizes 700+ IDNs based on these characteristics. The IDNs are positioned on the maturity scale as shown in the Figure 3.
Once categorized by their sophistication in managing and controlling care delivery, each system’s full network can be sketched out with sites of care, provider practices, and individual health care provividers under management. This step is vital to ascertain the scale and the level of control the health system exhibits in the local market.
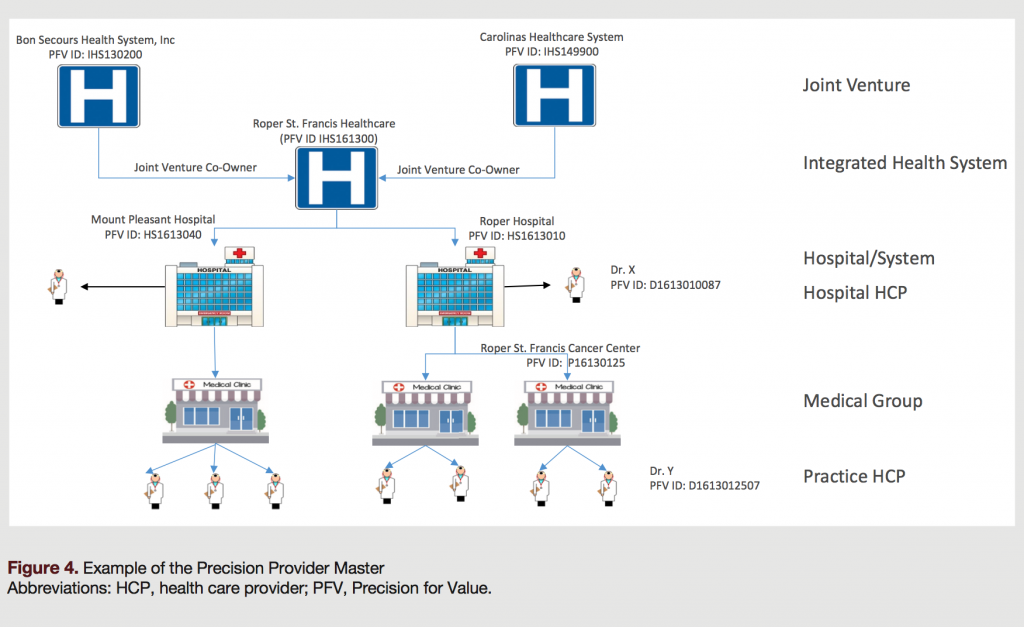
To better understand the total IDN network, Precision’s Provider Master is a tool that offers a turnkey, data vendor-agnostic, employment, ownership, and relationship map of the health care providers across the country. The Provider Master is displayed in a multilevel hierarchy that enables the unmasking of corporate decision-making and its impact on health care delivery (Figure 4).
Key Findings
What we have observed through our model is that the impact of high-control health systems on local market care delivery is positive and nonlinear. In addition, the influence of these systems has a significant spillover impact on the total health care delivery within the local markets in which they operate. This is critical to understand, as the drivers and levers of these systems, and the engagement model with these stakeholders (ie, partnerships, promotions, and contracts among stakeholders) have an effect not only within that health system but also on the overall local market. This impact has been identified as an influencer of many variables related to the provision of care, including but not limited to: (1) provider and channel contracting; (2) uptake of innovative treatment strategies; and (3) payer influence within the market.
Conclusion
For payers looking to expand partnerships with IDNs, oncology care providers competing in local markets, or pharmaceutical manufacturers looking to launch new products/indications or designing go-to-market strategies, it is vital to keep in mind that:
- the more fragmented the care, the lower the resistance to influence a local market;
- contracts with providers in network of sophisticated IDNs need to be modeled at the local market level, in context of all the stakeholders, to understand the true impact they can achieve;
- the higher the spread of high-control health systems in a local market, the lower the deviation in oncology care management; and
- quantify before you qualify, ie, model the impact of the system(s) before conducting research to address
the “why.”
References
- Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. 2009;27(17):2758-2765.
- The Dartmouth Institute. The Dartmouth Atlas of Health Care. Dartmouth Atlas website. http://www.dartmouthatlas.org/. Accessed February 7, 2018.
Citation
J Clin Pathways. 2018;4(1):39-41. doi:10.25270/jcp.2018.02.00004