Unlocking the Medical Payer Master
By Ashwin Athri
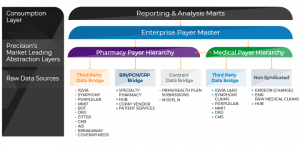
Over the past few years, pharmaceutical manufacturers have launched an increasing number of products covered under a health plan’s medical benefit. In response, health plans are exploring applying tools used successfully on the pharmacy benefit to the medical benefit. Correspondingly, there are increasing number of data vendors providing real-world evidence (RWE) data with medical claims information to support pharmaceutical manufacturers analysis of medical policy contracting scenarios, patient journey, patient finding, total cost of care and other such advanced insight-mining activities. These analyses should increasingly incorporate a comprehensive representation of the health plans, their attributes, and the ability to link the medical claims to the drug utilization management.
Traditionally, both data vendors and downstream warehousing systems have focused on understanding and organizing the pharmacy benefit, then applying that mastering clumsily to the medical benefit. The pharmacy benefit approach focused on pharmacy benefit managers (PBMs), employers, unions, prescription drug plans (PDPs) and other such entities forming a part of the payer universe that are not relevant in medical benefit management.
Digging a bit deeper, it becomes clear that RWE data sources have nonstandard payer identifiers, as they have plan names and plan IDs that are sourced directly from the billing systems and clearing houses. As there is no NCPDP [BIN/PCN/GROUP] equivalent identifiers in the medical payer definitions, there is no set standard across the systems and payers that the information is collected from. This poses an additional challenge when it comes to mastering the payer dimension across data sources that are not from syndicated data providers.
To solve for these and other challenges posed in representing the medical payer, Precision has developed a Medical Payer Master product with bridge files for the syndicated and RWE data sources. The Medical Payer Master has ~1,900 health plans (620 Commercial, 200 Health Exchange, 540 Medicare and 550 Medicaid) that cover all the medical lives in the US. This Master has corresponding bridge files to all the syndicated claims and medical coverage data sources in the marketplace.

More importantly, Precision has developed a map from the clearinghouse and billing system payer ID and payer names to the Master. This helps uncover the Payers in the RWE data sources and allows the user to connect it to other syndicated sources to have a uniform view of the payer. This unlocks the richness in the patient-level analytics.
Equipped with this capability, analysts can now uncover the payer insights hidden in the data sources and unlock payer-patient–level insights such as medical policy impact on biologic utilization, payer total cost of care, patient stratification by plan type and others that were previously either time and/or cost prohibitive.
Come explore this solution with Precision, and unlock the hidden payer insights in your RWE data.